If This Is the Easy Way Out, I Want A Refund
PCOS, Ozempic, and the invisible toll of being everyone’s unsolicited health project.
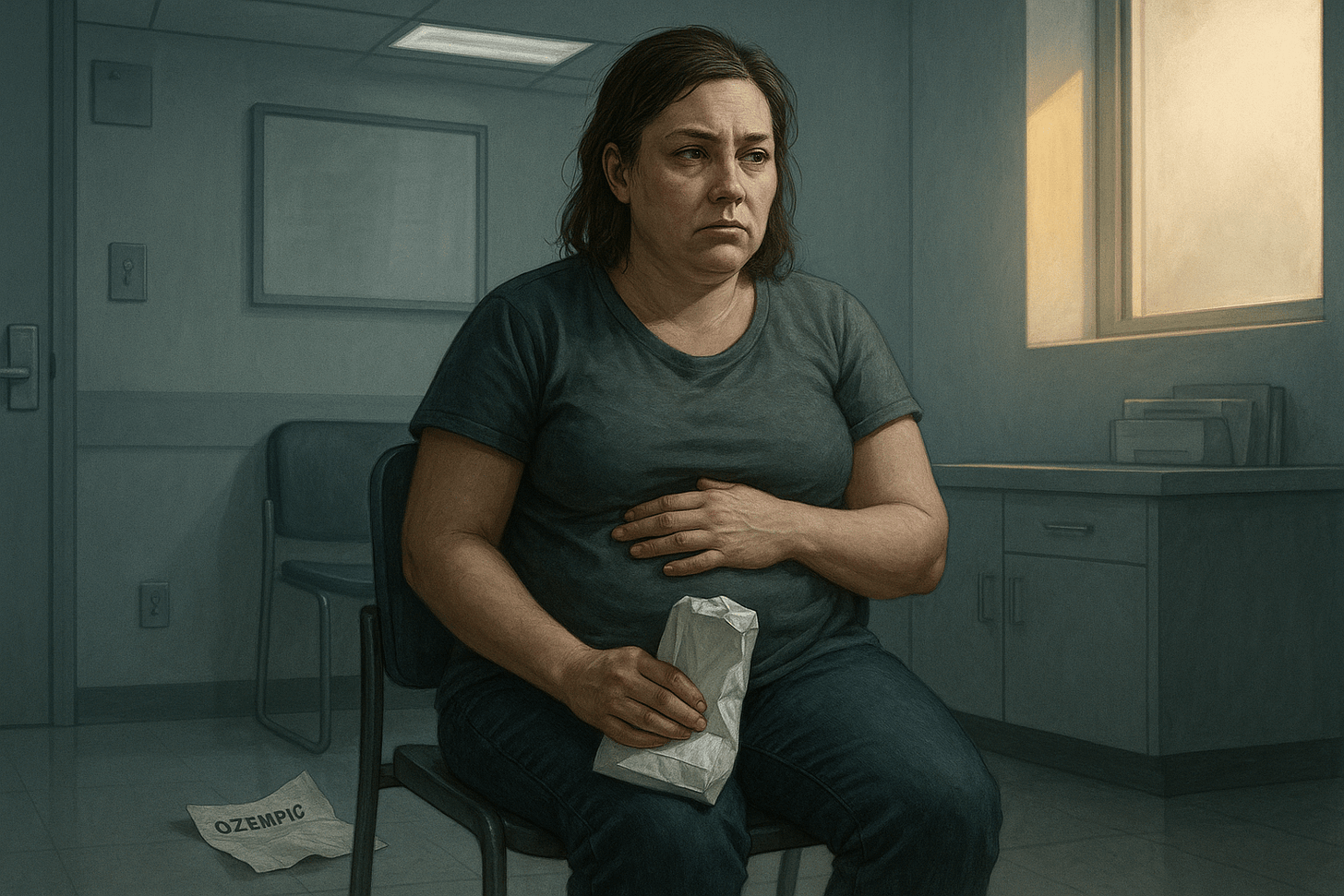
Hope in a Syringe
I started Ozempic in September. I didn’t tell many people at first, mostly because I was afraid of what they’d think.
There’s so much judgment around it. People think you’re cheating. That you’re taking the easy way out. That you’ve given up or sold out or poisoned yourself with chemicals just to lose weight. And truthfully? I don’t love medication either. I wish I didn’t need it. I wish I didn’t have to navigate this mess at all.
But I live in a body with PCOS. With stubborn insulin resistance. With a history of binge eating disorder. And after gaining 30 pounds on hormone therapy and hitting my highest weight ever, I was desperate for relief. Not thinness. Not a perfect body. Just some kind of steadiness inside my own skin.
At first, I felt hopeful. The cravings quieted. My appetite leveled out. I was losing weight slowly, gently. I thought I’d finally found something that worked with my body, not against it.
Then the dose increased.
And everything changed.
When the Miracle Backfires
The weight loss slowed. Then stopped. Then reversed. And with it came something I didn’t expect:
Primal, urgent sugar cravings.
Not just hunger. A wild, panicked, obsessive need for sugar, especially in the evenings. The kind of craving that hijacks your whole body. I couldn’t focus. I couldn’t stop thinking about it. I wasn’t just craving sugar; I felt like I needed it to survive.
And the emotional toll? It wrecked me. I became afraid to eat anything. My health anxiety kicked into overdrive and convinced me that every bite I took was going to kill me. I spiraled. I couldn’t sleep. I couldn’t trust my own body. And when the scale started creeping back up, I fell apart.
I have made big dietary changes. Upped my protein. Cut back on carbs. I have done all the things.
And still, I gained weight. Again.
And the worst part isn’t even the weight gain.
It’s the judgment.
People started asking if I was still doing Weight Watchers. If I was “sticking to the plan.” Like I was cheating. Like I was lazy. Like I wasn’t trying hard enough. Because in their minds, I was taking a weight loss drug, the miracle drug. I should be melting.
But that’s not what has been happening.
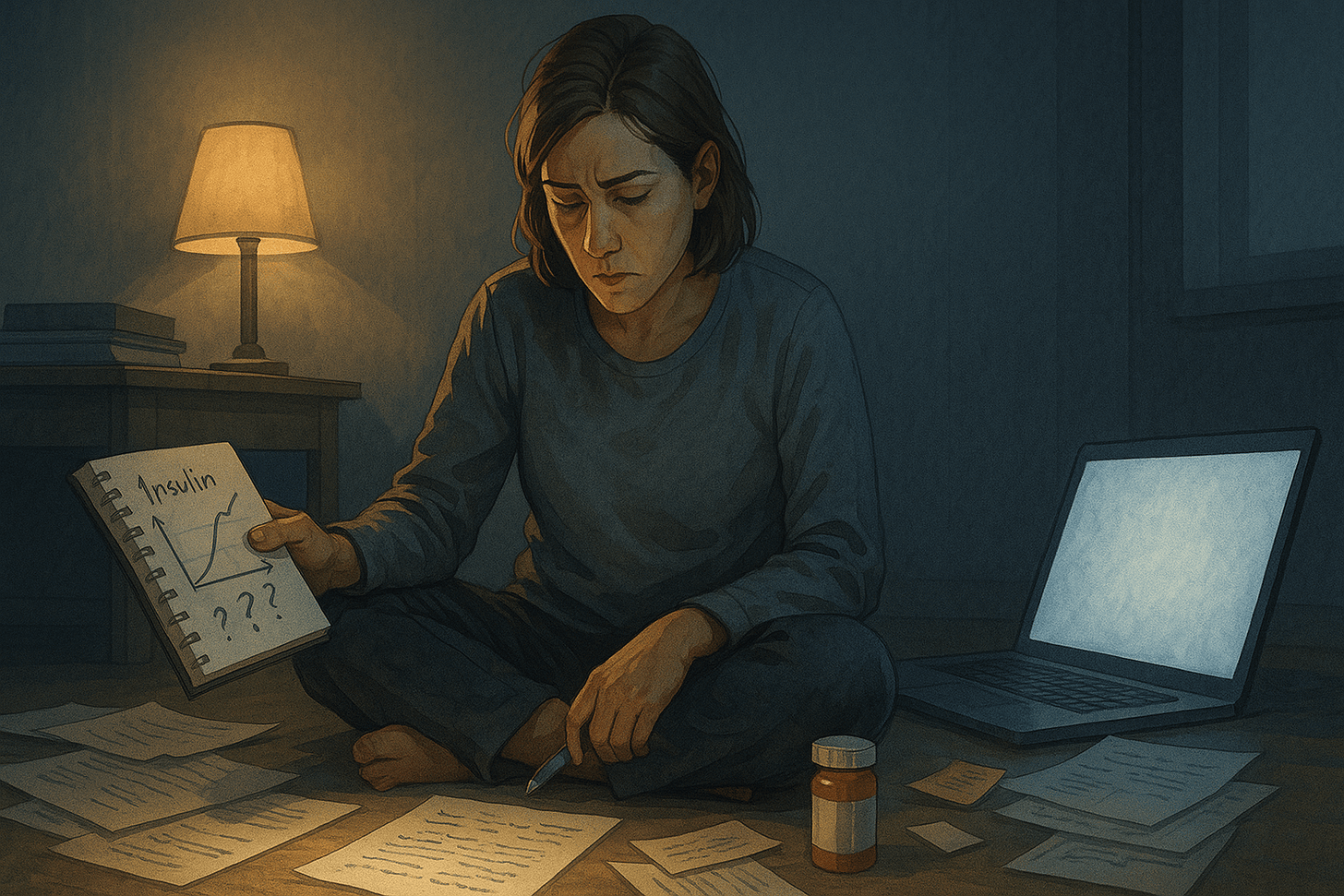
Science, Actually
In April, I had bloodwork done. Most of my labs looked better than ever. But my fasting insulin had skyrocketed.
I knew that was likely what was causing the cravings, the weight gain, the spiraling. But when I showed the results to my provider, she said, “I’m not worried about it.”
I left feeling dismissed.
Now, I like her. She’s been supportive in a lot of ways. But I don’t think she knew what to do with that data. And maybe she didn’t mean to invalidate me, but she did.
And I know my body. I’ve lived in it for 47 years. I know when something is off.
Then, last week, I was talking to a new friend who also has PCOS and had started Ozempic. Turns out she was experiencing the exact same thing: intense sugar cravings and slow to no weight loss. That got me thinking, and I did what I do best. I dove into the research, and what I found made me both furious and validated.
Here’s what was likely happening:
In some people with PCOS and insulin resistance, Ozempic can actually overstimulate insulin production, especially at higher doses. After a meal, glucose drops fast, but insulin stays high. The brain reads that as danger, triggering a release of hormones like cortisol and adrenaline to correct the imbalance.
It’s like slamming the brakes on your blood sugar while your insulin is still flooring the gas pedal. Your body spins out trying to balance itself, and the crash leaves you desperate for sugar.
It isn’t about willpower, it’s survival physiology.
And here’s the kicker: for someone like me, someone whose nervous system is already wired to scan for danger, whose health anxiety keeps every symptom under surveillance, this kind of misfired metabolic panic doesn’t just feel physical. It feels existential.
My body isn’t just saying “feed me.” It’s saying “fix this or you will die.”
Subscribe and join me for real talk about, grief, shame, and healing.
Let’s Talk About Shame
I’ve carried shame around food my entire life. Not just mild embarrassment, but a bone-deep belief that something was wrong with me. Something I needed to hide.
Growing up fat in a world obsessed with thinness, I internalized the idea that every bite I ate was evidence of failure. And the thin people around me? They didn’t question the system. They just assumed I could eat less, and the weight would fall off.
That’s not how PCOS works. That’s not how binge eating disorder works. That’s not how my body has ever worked.
That shame? It calcified. It turned into secrecy, into guilt, into a deep self-loathing that colored every food choice.
Every salad wasn’t health, it was penance.
Every craving wasn’t just a craving, it was a moral failing.
Every binge was followed by days of mental punishment.
And the shame of not being "successful" on Ozempic? That layered it even thicker.
The shame of needing help.
The shame of not responding the way I was “supposed to.”
The shame of gaining weight on a weight loss drug.
You can’t logic your way out of that kind of shame. You can only drag it into the light and say, “Look, it’s here. And I’m still standing (barely).”
To Those Who Think They Know Better
Before I go full throttle here, let me say this gently, especially to those who care but don’t quite understand:
Some of you have never lived in a body like mine. And that’s okay. Yet, if your first instinct is to offer advice, assumptions, or that one podcast your cousin loves, pause. Please. Just listen first.
I’ve wanted it so badly I’ve cried over it. Starved over it. Prayed over it. I’ve given up entire months of my life to tracking, weighing, calculating, restricting, and punishing myself, only to be told I should “just try harder.”
Start asking:
“How can I support you?”
“What do you need right now?”
“Do you want to talk about it?”
Because unless you’ve lived in a body that resists every effort…
Unless you’ve faced judgment at every turn…
It’s hard to understand what that does to a person.
So maybe, before offering advice, start with listening.
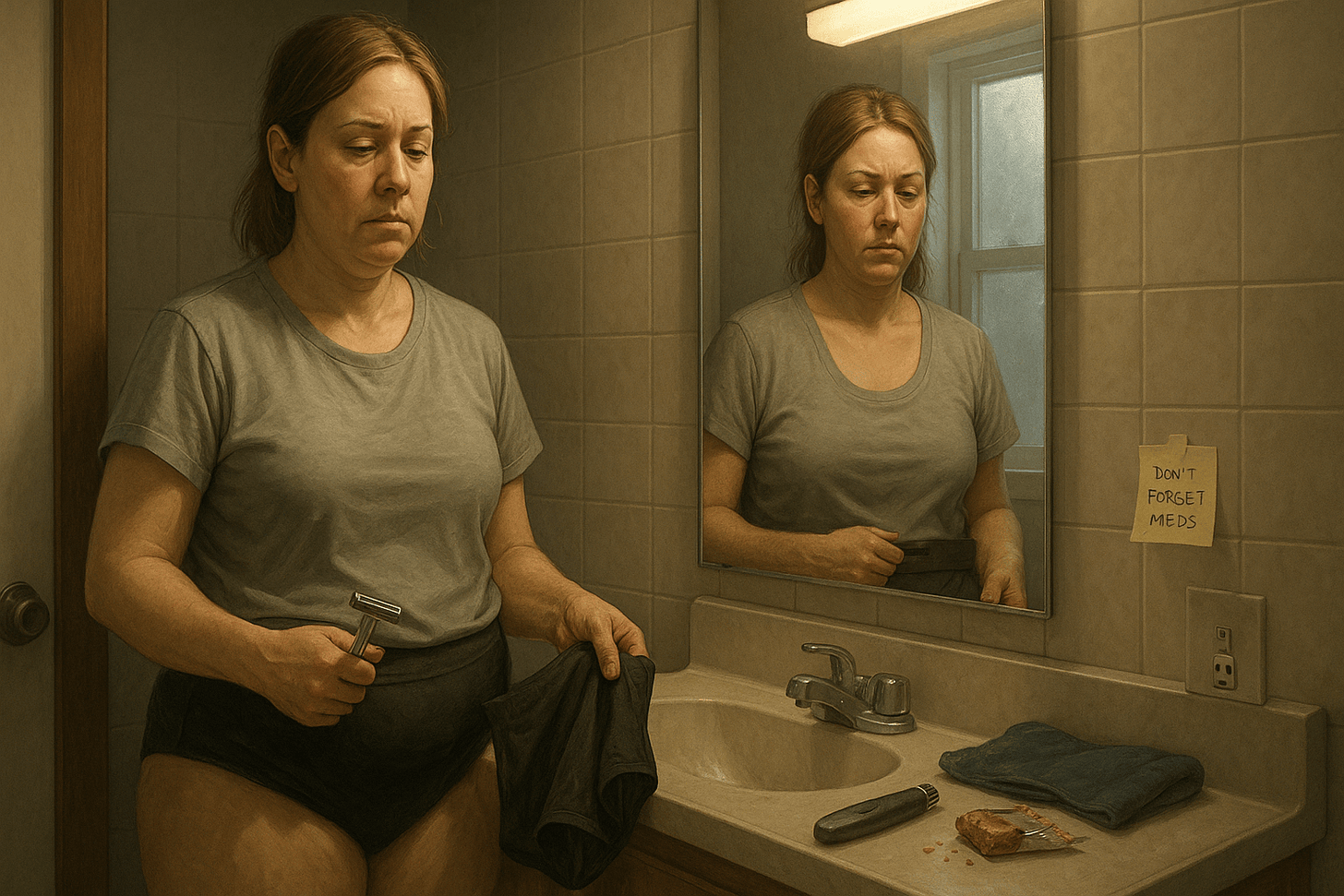
The PCOS Tax
PCOS is more than irregular cycles and weight gain. It’s bloating, brain fog, fatigue, mood swings, facial hair, hair loss, shame, infertility, and the invisible math we do all day just to get through.
We shave our faces before Zoom calls. We plan outfits around discomfort. We cancel plans because some days, just existing takes all our energy.
And when we do ask for help, we’re often told we’re just not trying hard enough.
But here’s what they don’t know:
There’s science showing that, for some of us with PCOS, Ozempic can backfire. It can overstimulate insulin, drop our blood sugar too fast, and set off a hormonal alarm bell that feels existential. Not “I’m craving cookies,” but “I feel like I’m going to die if I don’t eat sugar right now.”
This piece isn’t just about the meds.
It’s about the shame.
The isolation.
The mental toll of being gaslit by your own body, and by people who think they’re helping.
What I Want the World to Know
I want doctors to stop assuming and start listening.
Ask questions. Believe your patients. Research the things we already know about our own bodies. Don’t write us off because our numbers look “okay.” Don’t blame every symptom on weight. Don’t ignore patterns just because they don’t fit your expectations. You have so much power. Use it wisely. We are not difficult. We are not dramatic. We are not noncompliant. We are tired of being dismissed.
To our well-meaning thin friends, and friends who have an “easy” time losing weight: Please don’t make our bodies your curiosity project. Don’t ask us to explain ourselves or your cousin’s results. Just listen. Just be there. That’s enough.
To my fellow PCOS warriors who’ve found relief: If Ozempic worked for you, I’m genuinely happy for you. Truly. But please hold space for those of us it hasn’t helped. We are not your cautionary tales. We are not your failures. We’re simply walking another version of this complex, exhausting path. Don’t let your success erase someone else’s pain. (And don’t let their pain diminish your success.)
And to everyone else?
Stop assuming we haven’t tried.
Stop offering advice like we haven’t already Googled it hundreds of times.
Stop making our health your moral playground.
Try this instead:
Instead of “Have you tried…”, say “That sounds hard. I’m here.”
Instead of “Just lose weight,” ask “How can I support you right now?”
Instead of judging our plates, ask why you feel entitled to our bodies.
What Healing Looks Like (For Now)
So where do I go from here?
This week, I made a decision: I’m lowering my dose and pairing it with Metformin.
Not because anyone told me to. But because my body asked me to.
I’m not chasing weight loss anymore. I’m chasing peace. A steady nervous system. Fewer crashes. More clarity. I’m letting my providers support me, but I’m leading the way.
This isn’t a success story. Not yet.
It’s a reclamation. The beginning of one.
It’s the story of a woman who stopped outsourcing her knowing.
If You’re Still in It
If you’re reading this and nodding through tears or rage or both, please hear me:
You are not crazy.
You are not lazy.
You are not broken.
You are a person with a complex body and a fierce heart, doing your best in a world that keeps trying to shrink you.
And if no one’s said it to you lately…
Your body is not the problem. It never was.
Love today,
Heather 🌸